This is my story, in sharing I hope to create space for open conversations on women’s health.
I want these to be honest and transparent, focusing on aspects often dismissed, delayed or ignored.
The Wider Context: Women’s Health in the UK
Before I delve into my own experience, it is important to step back and consider the broader landscape of women’s health in the United Kingdom.

Gender Gaps in Medical Research
- The UK ranks 104th worldwide for the gender health gap.
- Although women live longer than men, we spend on average, three extra years in poor health.
- We constitute 51% of the population. Despite this, we have historically been underrepresented in clinical trials. Male data often serves as the default reference.
Research Bias and Under representation
- A significant number of studies continue to sidestep female physiology, commonly attributing this to “variability” caused by menstrual cycles.
- Critical conditions like menopause, endometriosis, and fibroids stay severely under-researched.
- Even for diseases that affect both sexes, like heart disease and dementia, sex-specific data is often absent. This absence results in misdiagnoses and substandard treatment for women.
Pregnancy and Childbirth
- Pregnancy-related conditions get minimal attention in clinical trials; a pattern partly rooted in longstanding bans after the thalidomide tragedy. Thalidomide scandal – Wikipedia
- Systematic failures in listening to women who have been harmed by medical devices and pharmaceuticals.
- Women, particularly those from ethnic minority backgrounds, routinely experience delayed diagnoses and inadequate care after complications related to childbirth.
Women’s health outcomes: Is there a gender gap? – House of Lords Library
Causes of the Health Gap
According to the LSE Public Policy Review – The gender health gap in the UK has multiple causes. It stems from systemic issues, socioeconomic factors, and behavioural aspects. These factors lead to poorer outcomes for women. Historically, medical research has centred on male biology, leaving women underrepresented in clinical trials and under served in care.
Conditions like endometriosis affect 1 in 10 women. They face an average diagnostic delay of seven years. This delay causes prolonged suffering and high healthcare costs. Polycystic Ovary syndrome (PCOS) and menopause related issues are similarly neglected in research and policy. This bias limits the development of effective treatments. It restricts access to accurate health information. These factors shape how and when women seek care.
Barriers to Women in Accessing Healthcare in the UK – A Review | LSE Public Policy Review
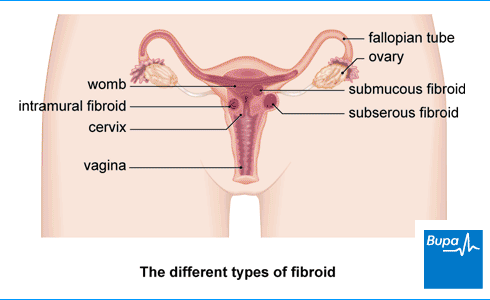
Fibroids – Breaking the Silence
In 2016, it was during a routine pregnancy ultrasound scan that I was first introduced to my fibroids. At that time and according to the medical advice they did not interfere with the pregnancy. As a result, no further action beyond monitoring was discussed. No treatment or management plans was discussed nor was a referral to a gynaecologist considered. My pregnancy ended prematurely, my son was born sleeping with no clear medical explanation on what had caused this. It was then I first began to realize how rarely these matters are studied. I also noticed how much is left to chance in women’s reproductive health.
In 2018, I became pregnant again, but this time we had a safeguarding plan in place. The fibroids remained and the medical advice about them stayed the same with my last scan in 2019. Thankfully, my son was born safely. Still, in the years that came after, I repeatedly flagged as anaemic after separate visits to the GP. I endured years of monthly heavy bleeding and a range of unexplained symptoms. Yet, the fibroids were never investigated further. No one connected the dots and no one pursued the why.
the Pursuit of Answers
Reflecting on my experiences, I had always assumed I was simply a “heavy bleeder.” Yet, after speaking with a few women, I realised that my periods were not just heavy they were extreme.
- Using super plus tampons alongside maternity pads.
- Needing to change protection every two to three hours during the first 48 hours.
- Feeling utterly exhausted yet still carry on as normal.
One described my symptoms back to me as “insane.” For me, they had been my normal for a very long time.
Earlier this year, feeling a solid mass in my lower abdomen sounded a very loud alarm. It prompted me to contact my GP but also took control of the situation.
I had done some of my own research. I was determined and armed with the full lists of issues. I was clear in my need for answers.
Investigations and Referral
After a new ultrasound scan and blood tests, I was flagged as extremely anaemic and prescribed high-dose iron tablets. The scan showed:
- The fibroids had grown since 2019.
- At least seven fibroids (intramural and subserosal)
- An enlarged uterus with irregular outline.
After nine years of living with fibroids I was finally referred to a gynaecologist.
The first try at a hysteroscopy under local anaesthetic was unsuccessful. This led to the scheduling of an in patient procedure under general anaesthetic.

What Is a Hysteroscopy?
A hysteroscopy is a medical procedure used to examine the inside of the uterus. A thin, lighted tube with a camera is inserted through the vagina. This eliminates the need for any incisions. The procedure allows doctors to visualise the uterine cavity and detect any abnormalities.
Reasons for Performing a Hysteroscopy
- Investigating the cause of heavy or irregular menstrual bleeding.
- Diagnosing and treating fibroids, polyps, or scar tissue within the uterus.
- Exploring underlying reasons for infertility or recurrent miscarriage.
- Removing a displaced intrauterine device (IUD) or obtaining tissue biopsies.
Reasons for Performing a Hysteroscopy
- Investigating the cause of heavy or irregular menstrual bleeding.
- Diagnosing and treating fibroids, polyps, or scar tissue within the uterus.
- Exploring underlying reasons for infertility or recurrent miscarriage.
- Removing a displaced intrauterine device (IUD) or obtaining tissue biopsies.
It can be carried out under either local or general anaesthetic.
When Is General Anaesthetic Required?
- Presence of large fibroids or polyps.
- Extensive scar tissue within the uterus.
- Abnormal uterine shape.
- Suspicion of malignancy.
Treating Fibroids
I went looking for information on the available treatments for fibroids.
Below are the main approaches I found:
1. Medical Management
- Hormonal therapies, including small doses of progesterone in contraceptive approaches, can help to reduce bleeding and pain. Yet, the long-term sustainability of these treatments; their impact on fertility remained a concern for me.
- Tranexamic acid or non-steroidal anti-inflammatory drugs (NSAIDs) are used for symptom relief.
- Gonadotropin-releasing hormone (GnRH) agonists are sometimes prescribed to temporarily shrink fibroids, often before surgery.
2. Minimally Invasive Procedures
- Uterine Artery embolisation (UAE).
- MRI-guided focused ultrasound (MRgFUS).
- Endometrial ablation destroys the uterine lining (not suitable for those wishing to preserve fertility).
3. Surgical Options
- Myomectomy, which involves removing fibroids while preserving the uterus.
- Hysteroscopic resection, suitable for fibroids located within the uterine cavity.
- Hysterectomy, the total removal of the uterus.

The Verdict
When I woke up after the hysteroscopy, I was hopeful. I expected a clear and positive plan of action. However, the reality was quite different.
I received one option I was dreading the most. a hysterectomy.
- My fibroids are too embedded and scattered to remove without harming the uterus.
But my ovaries would be fine, they said but yes, a hysterectomy!
What Is a Hysterectomy?
A hysterectomy is a major surgical procedure that involves removing the uterus. Depending on the specific type, the surgery may include removal of the cervix. It can also involve removing the ovaries, fallopian tubes, and surrounding tissues.
“A hysterectomy is a major operation with a long recovery time and is only considered after less invasive treatments have been tried.”
Still Entangled
I find myself grappling with a mix of emotions and unanswered questions.
I am facing the prospect of a hysterectomy as my only medical option to remove fibroids. I wonder if I have all the necessary information and tools. This would help me make an informed decision.
- Why did it take nearly a decade to reach this critical juncture?
- Is a hysterectomy my only choice? This is typically considered as a last resort.
It makes me question whether timely referrals may have allowed me to plan differently. Having full access to my medical records is crucial, as is seeking a second opinion.
The most challenging question: am I truly ready to face life without my uterus?
the UK’s Current Position
The Women’s Health Strategy for England, published in 2022, aimed to transform approaches to women’s health.
https://www.gov.uk/government/publications/womens-health-strategy-for-england
While the strategy has laid vital groundwork, continued investment and accountability are essential to closing the gender health gap.
Three years in, notable progress has been made but key challenges persist.
A Work in Progress: Evaluating the Women’s Health Strategy | RCOG
If you’ve been through something similar or know someone who has, I hope this helps you feel seen.
And if you’re in healthcare, policy, or research please, let’s do better.

Leave a comment